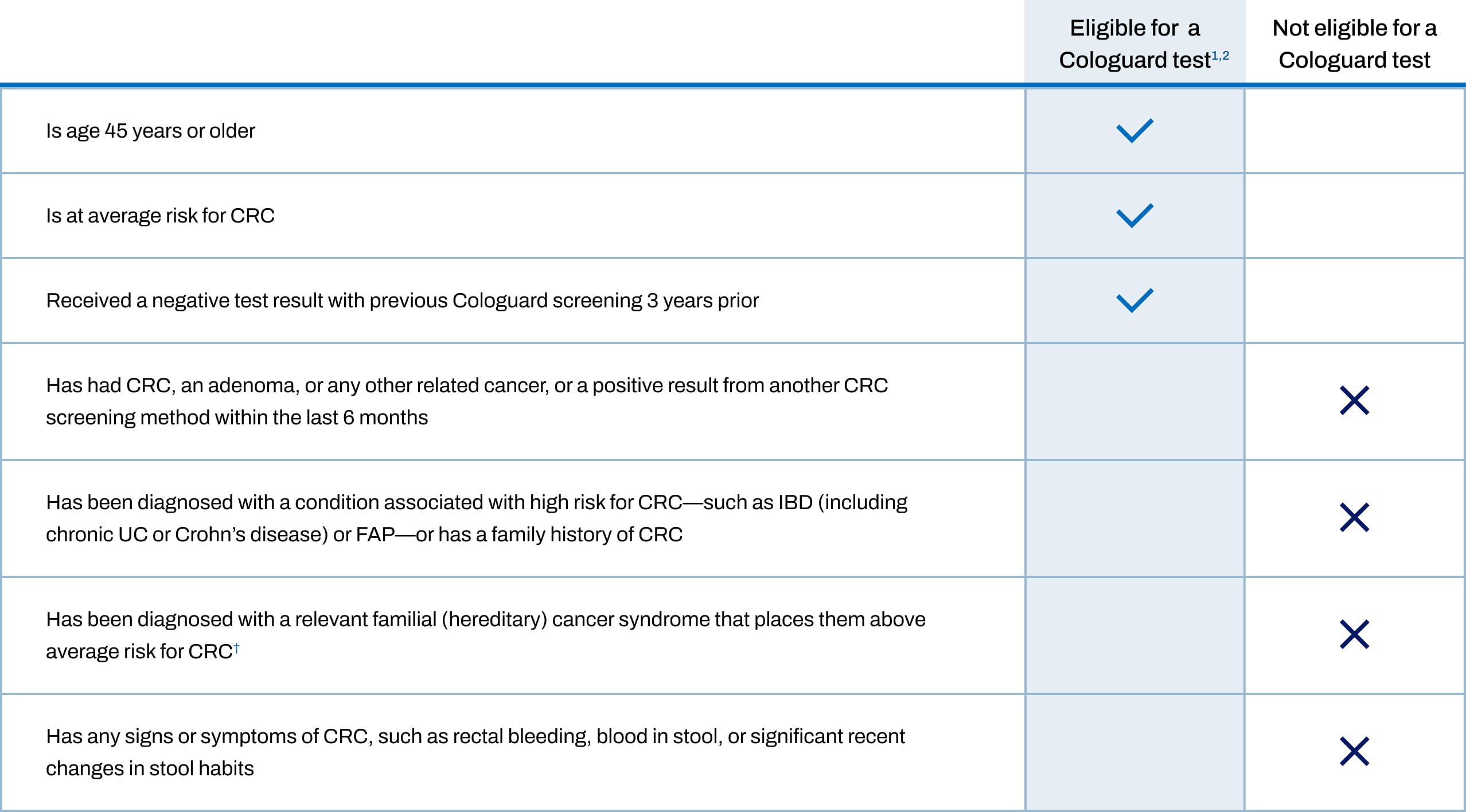
PATIENT ELIGIBILITY
Offer the Cologuard® test to every eligible patient aged 45 and older at average risk for colorectal cancer (CRC)1,2
For over 10 years, over 380,000 healthcare providers have trusted the Cologuard test to screen over 15 million patients.3,4*

Which patients receive the Cologuard Plus™ test vs the Cologuard test?
Eligibility criteria for both tests are the same. Exact Sciences will determine which test your patients receive based on which test their insurance covers.
- Data as of January 31, 2025.3
- Such as hereditary nonpolyposis CRC syndrome (or Lynch syndrome), Peutz-Jeghers syndrome, MYH-associated polyposis, Gardner’s syndrome, Turcot’s (or Crail’s) syndrome, Cowden’s syndrome, juvenile polyposis, Cronkhite-Canada syndrome, neurofibromatosis, or familial hyperplastic polyposis.1,2
- For patients with traditional Medicare, a colonoscopy after a positive Cologuard result is still a screening colonoscopy based on updated Centers for Medicare & Medicaid Services regulations, effective January 1, 2023. Medicare does not apply cost sharing to screening colonoscopy. This update does not apply to commercial plans with exempted status.5,6
FAP=familial adenomatous polyposis; IBD=inflammatory bowel disease; UC=ulcerative colitis.

